Skin Imaging for Non-Dermatology Researchers: What You Need to Know
Posted on
Skin Imaging for Non-Dermatology Researchers: What You Need to Know
If you’re working in immunology, oncology, or wound healing, skin is more than just a surface. It can serve as a biologically meaningful read-out, revealing insights into inflammation, healing, drug responses, and more.
This shift may feel new. Many researchers weren’t trained to interpret skin-imaging data or evaluate devices, so below is a fast-track guide to what skin imaging can do for your research and why it matters.
What Skin Data Can Actually Tell You
Beyond the Surface: Why Skin Is a Window into Biology
Skin is often overlooked in non-dermatology research, but it’s a powerful tool for understanding complex biological processes. Here’s how skin biomarkers can provide valuable insights:
- Hydration & barrier function: assesses immune responses, inflammation, and topical-treatment efficacy.
- Pigmentation & melanogenesis: signals systemic changes, including drug responses and metabolic shifts.
- Elasticity & extracellular matrix: tracks collagen synthesis and wound healing, informing tissue-regeneration or tumor-progression studies.
When working with skin imaging in preclinical studies, the value lies in how those skin changes reflect broader systemic processes or responses to treatments. For example:
- Immunology: early skin inflammation (erythema, edema) can foreshadow systemic immune flare-ups.
- Oncology: skin endpoints help gauge drug response in cutaneous tumors and illuminate tumor-microenvironment shifts.
- Wound healing: elasticity, hydration, and tissue-regeneration metrics predict how well the body is repairing itself.
- Drug absorption: imaging-based changes in hydration, pigmentation, or elasticity can reveal how effectively a topical drug is being absorbed.
The Methods You Might Be Using and Their Limits
Visual Grading and Calipers Aren’t Enough Anymore
Many researchers still rely on subjective methods like photos, manual scoring, and caliper measurements
However, these tools have limits:
- Subjectivity: manual scores drift between researchers (and even within the same researcher over time).
- Low reproducibility: inconsistent placement erodes longitudinal accuracy.
- Lack of depth/resolution: photos and calipers miss subsurface structures such as collagen or vasculature.
That’s where imaging comes in. Objective, reproducible imaging standardizes assessments and delivers quantifiable results, saving you from the $9.99 Amazon caliper (we’ve all been there).
Skin-Imaging Tech 101: No Jargon Needed
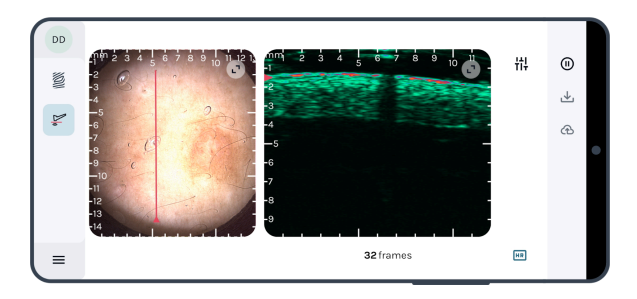
This advanced SkinScanner tool delivers comprehensive insights into skin health, allowing researchers to track and quantify changes in hydration, pigmentation, elasticity, and more with accuracy.
A quick, researcher-friendly breakdown of imaging options:
- SkinScanner: handheld, ultra-high-frequency ultrasound (20–40 MHz, ≤ 10 mm depth) with dermoscopy guidance for rock-solid repositioning and high-resolution dermis mapping.
- Dermoscopy: surface-level imaging for lesions, vascularity, and texture.
- Ultrasound (conventional): visualizes deeper layers for tissue-density and structure insights in oncology or wound studies.
- 3D imaging / OCT (optical coherence tomography): combines surface and subsurface views at high resolution for detailed tissue analysis.
Match the modality to your research question so you capture the data you need—no more, no less.
Choosing the Right Tool-Key Questions to Ask
- Reproducibility: Can you position and scan the same region each time? If sub-millimeter repeatability matters, a built-in positioning line can trump headline MHz. Kent’s SkinScanner couples 40 MHz ultrasound with dermoscopy guidance, so you can rescan day-3 and day-7 lesions in the same footprint.
- Resolution: Cellular detail or broader tissue view?
- Ease of use: Will techs, PIs, and students all be productive on day one?
- Data handling: Does the system annotate, compare, and export pain-free?
- Compatibility: Will it slot into existing workflows, sample types, and analytics?
Answering these questions helps you choose a fit-for-purpose system without unnecessary complexity or cost.
The Bottom Line
You don’t need to be a dermatology expert to collect solid skin data. With the right tools, skin imaging becomes a repeatable, quantifiable part of your research whether you’re tracking wound healing, assessing drug responses, or exploring tissue regeneration.
If you’re exploring skin endpoints for the first time, we’re happy to walk you through what’s possible.