TLDR: This article explains how to choose an oxygen concentrator for small animal anesthesia and recovery. Sizing is more about flow demand and workflow, and less about animal size. It covers typical mouse/rat/rabbit flow ranges, why leaks and “spike” needs (flushes, induction, recovery) matter, and when 5 L/min vs 10 L/min makes sense. It also stresses monitoring (pulse oximeter), warming, and that oxygen supply isn’t ventilation.
Choosing Small Animal Oxygen Concentrators
If you’re shopping for an oxygen concentrator for small animals in a research lab or veterinary setting, you’re not trying to help Grandpa binge-watch cable TV. You’re trying to keep animals stable during anesthesia and recovery, reduce cylinder swapping, and make your anesthesia workflow less fragile.
This guide helps you size a concentrator for mouse/rat work up through rabbits and similar species—without hand-wavy “it depends” advice.
We’ll cover flow demand, what “oxygen purity” really means, backpressure and plumbing realities, how concentrators fit into anesthesia delivery (including isoflurane), and what else belongs in the setup (mask or intubation gear, monitoring, and sometimes ventilation).
Let’s look at what an oxygen concentrator actually is
An oxygen concentrator pulls in room air and uses a sieve/adsorption process to deliver oxygen-enriched gas. Most units deliver their highest oxygen concentration at lower flow rates, and concentration may decrease as you push them toward max output. Exact performance varies by model, age, oxygen concentrator filters, maintenance, altitude, and downstream restrictions.
In animal research and veterinary use, concentrators typically serve one (or more) of these roles:
- Carrier gas source for inhalant anesthesia (commonly isoflurane)
- Supplemental oxygen during sedation/anesthesia and recovery
- Convenience + redundancy so you’re not tied to cylinders 24/7 (and your O2 source isn’t tied to a wall!)
Key point: a concentrator is an oxygen source. It is not a ventilation strategy, not a leak-fixer, and not a guarantee that an animal is oxygenating well (that’s what monitoring is for).
The real sizing problem is flow rate, not animal size
People assume “small animal = tiny flow.” That’s how you end up with an oxygen concentrator for small animals that looks fine on paper and falls apart on a busy day.
Your required flow is usually driven more by:
- the anesthesia circuit type
- mask leakage
- scavenging setup
- how many stations you run at once
- workflow spikes (flushes, induction box, recovery hood, etc.)
So yes, species matters—but your equipment + habits often matter more.
Two different use cases that change the math
1) Oxygen as part of anesthesia delivery
Flow depends on the circuit, vaporizer/system design, and whether you’re doing genuinely low-flow vs turning it up because you didn’t realize there was a leak in your line (oops!)
2) Oxygen for recovery/support
Flow depends on the delivery method (cage flow-by, hood, chamber, mask support, etc.) and how many animals you’re supporting concurrently.
Same concentrator. Totally different demand profiles.
Step 1: Define your use case (don’t skip this)
Before you compare models, answer these clearly:
A) What are you actually doing?
- Mask anesthesia for mouse/rat?
- Rabbit/guinea pig anesthesia?
- Recovery support only?
- Any cases requiring intubation (endotracheal tube = a tube placed in the airway)?
- Any cases requiring ventilation (mechanically moving gas in/out of lungs)?
B) How many animals/stations at once?
- One animal at a time
- Two anesthesia stations
- Induction + maintenance + recovery happening simultaneously
C) What’s your circuit reality?
- Non-rebreathing (common for rodents)
- Rebreathing (more common as animal size increases)
- If you can actually use low flow rates (great in theory, not so great if you need 10ft of tubing to send your animal into an MRI)
D) What does failure look like?
- Does a dip in O₂ output stop anesthesia?
- Does cylinder swapping interrupt procedures?
- Do you need redundancy (concentrator + backup cylinder)?
Write these down. This is where a lot of purchasing decisions go sideways.
Step 2: A practical sizing rule that works
1) Estimate continuous flow
Take your typical maintenance flow and multiply by the max number of stations you run concurrently.
Example:
- 1 rat station at 1.5 L/min → 1.5 L/min continuous
- 2 stations → 3.0 L/min continuous
2) Add headroom for leaks and reality
Add 25–50% margin.
Example:
- 3.0 L/min continuous → target 4.0–4.5 L/min capacity
3) Decide if spikes matter in your workflow
If you do frequent flushes, run an induction box, or support recovery flows at the same time, you want a system that doesn’t collapse under peak demand.
This is why many labs land on:
- 5 L/min as a baseline for single-station work
- 10 L/min when they run multiple stations, larger animals, or heavier workflow peaks
Step 3: 5 L/min vs 10 L/min—what actually changes
5 L/min concentrator is usually a fit for
- single-station mouse/rat mask anesthesia
- light recovery support
- low-to-moderate throughput workflows
Watch-outs:
- oxygen concentration may drop near max flow (model-dependent)
- less forgiving during spikes (flushes, splits, leaks)
- easy to outgrow
10 L/min concentrator is usually a fit for
- two stations running concurrently
- rat-to-rabbit anesthesia days
- higher-flow recovery support (or multiple recovery cages)
- labs that don’t want O₂ to be the bottleneck
Watch-outs:
- higher cost
- more space/noise (often)
- still not a ventilator, still not a substitute for good technique
Blunt truth: if you’re doing anything beyond single-station rodent work, 10 L/min is frequently the “buy once, cry once” choice.
Step 4: Concentration, pressure, and why oxygen concentrators disappoint people
Oxygen concentration isn’t constant
Many concentrators deliver their best concentration at lower flows and can drift downward as demand rises. For most small animal anesthesia workflows, the bigger practical questions are:
- Is output consistent during my typical day?
- Can it maintain flow under normal and peak conditions?
- Does the system behave predictably when split across stations?
Pressure and downstream restrictions matter
Concentrators are sensitive to your “plumbing”:
- long tubing runs
- quick-connects
- multiple splitters
- filters
- undersized tubing
- restrictive fittings
If your setup is a maze of adapters, you can create pressure drop and unstable delivery even with a perfectly good concentrator.
Practical rule: make the concentrator’s job easy. Shorter runs, proper tubing, fewer bottlenecks, clean filters.
Step 5: Using an oxygen concentrator with isoflurane anesthesia
Yes—often a concentrator can supply carrier gas for isoflurane anesthesia. But whether it works smoothly depends on the system design and how you run it day-to-day.
Mask anesthesia (non-intubated)
- common in mouse/rat workflows
- flow demands are usually manageable for single-station work
- mask leaks are common and drive higher flows (and increase exposure risk)
Intubated anesthesia (endotracheal tube)
Intubation changes your risk profile and your control:
- better airway control and often less leak
- requires correct tube sizing and technique
- may be paired with ventilation depending on the procedure
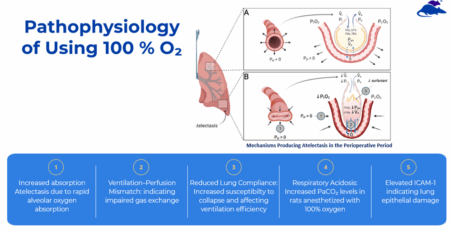
Ventilation (small animal ventilator)
A ventilator’s job is ventilation—moving gas in and out. Oxygen concentration is separate. Depending on the ventilator and how it integrates with your anesthesia setup, you may need to plan for:
- different flow demands
- different connection requirements
- greater need for stability and monitoring
If you have ventilation in your present or near future, don’t treat “oxygen source” as the whole plan. It’s one component in a bigger system.
Step 6: Monitoring isn’t optional (pulse oximeter at minimum)
Oxygen supply does not equal oxygenation. If you’re using oxygen in small animal anesthesia, you need a way to confirm you’re getting the outcome you think you’re getting.
Pulse oximeter basics:
- measures oxygen saturation as a trend (not a perfect truth machine)
- readings can be affected by motion, low perfusion, sensor placement, temperature, and anesthetic depth
Practical tips:
- use appropriate sensor placement for the species
- keep animals warm (see next section)
- treat oximetry as a trend + early warning, not a single magic number
Step 7: Heat support improves everything
Hypothermia is common during rodent anesthesia and it can wreck physiology fast. You can supply “perfect oxygen” and still get unstable outcomes if the animal is cold.
If you want smoother anesthesia and better recovery:
- prioritize warming and temperature monitoring
- make it part of the standard workflow, not an afterthought
Step 8: Oxygen concentrator setups that work in real life
Pattern A: Single-station rodent anesthesia + recovery
- 5 L/min concentrator
- mask anesthesia setup
- pulse oximeter
- heat support
- backup cylinder for downtime
Best for: typical mouse/rat work, one at a time
Pattern B: Two stations / higher throughput
- 10 L/min concentrator
- split to two stations with proper flow control
- scavenging that’s actually effective
- monitoring per station if feasible
- backup cylinder
Best for: labs doing lots of animals or running rat + rabbit days
Pattern C: Intubation-capable suite
- often 10 L/min class concentrator (sometimes plus cylinder backup)
- species-appropriate endotracheal tubes + intubation tools
- ventilation integration if the procedure requires it
- monitoring: pulse ox, temperature (and more as needed)
Best for: airway control workflows where you don’t want surprises mid-procedure
Step 9: Quick checklist before you buy
Use this to sanity-check your purchase:
- How many stations at once?
- Typical maintenance flow per station?
- Do you need spike capacity (flushes, induction box, recovery hood)?
- Mask only, or intubation too?
- Any ventilator integration now or in the next 12–18 months?
- Do you have leak control and scavenging handled?
- Do you have monitoring (pulse oximeter at minimum)?
- Do you have a backup plan for downtime?
- Where will it live, and who maintains it?
One more uncomfortable question: are you trying to solve a workflow problem with a hardware purchase? Sometimes the right answer is “fix the leaks and the process first.”
Simple sizing recommendations
- One station, mouse/rat mask anesthesia + light recovery → start with 5 L/min
- Two stations, heavier throughput, rat + rabbit days, higher recovery flows, or future growth → choose 10 L/min
- Intubation + ventilation plans → treat the concentrator as one piece of the system; design around the circuit + ventilator requirements, and still plan for monitoring and redundancy
No matter what: plan for leaks, monitor oxygenation, and don’t confuse “oxygen source” with “ventilation solution.”
Oxygen Concentrator FAQs
What size oxygen concentrator do I need for rodent anesthesia (mouse vs rat)?
Most single-station mouse/rat setups can run on a 5 L/min concentrator if your circuit is tight and you’re not splitting to multiple stations. If you run two stations, do higher-throughput days, or rely on flushes/recovery flow simultaneously, 10 L/min is usually the smarter move.
Can I use an oxygen concentrator as the oxygen source for isoflurane anesthesia?
Often yes—if the concentrator can maintain the flow and pressure your anesthesia setup needs. The limiting factor is frequently the circuit + leaks, not the animal.
Is a 5 L/min concentrator enough if I’m using an induction box or doing flushes?
Sometimes, but this is where people get burned. Induction boxes and flush habits create short spikes in demand. If that’s part of your workflow, a 10 L/min unit (or a concentrator plus cylinder backup) tends to be more stable.
Do I still need monitoring if I’m using an oxygen concentrator?
Yes. Oxygen supply doesn’t guarantee oxygenation. Use a pulse oximeter to track saturation trends, and keep animals warm to improve both physiology and signal quality.
Does an oxygen concentrator replace a small animal ventilator?
No. A concentrator provides oxygen-enriched gas. A ventilator provides ventilation (moving gas in and out). If the animal isn’t ventilating adequately under anesthesia, the solution is ventilation strategy—not “buy a bigger concentrator.”
Practical Next Steps in Choosing the Right Oxygen Concentrator
If you tell us (1) species (mice vs rat, etc), (2) number of stations, (3) whether you’re mask-only or intubating, and (4) what your busiest day looks like, we can sanity-check your flow assumptions and help you avoid buying the wrong class of concentrator for your anesthesia workflow.